Currently, different vaccines with different storage conditions are distributed among 150 vaccination centers in Belgium. The Think Tank Vaccine Distribution investigated which parts of the complex chain could be cut out to make the chain more effective. Or: How can we spare the already busy hub hospitals, and how can we minimize the loss of vaccines? Because the more complex the chain, the more vaccines could be lost due to miscounting, mishandling, etc.
“In logistics there is a universal law that states: the more intermediate steps, the more mistakes there can be statistically.”
Two scenarios
Healthcare personnel and hospitals have been under serious pressure. Currently, hospitals are still widely used as vaccine hubs. According to logistics theory, this is an additional and inefficient step. Our proposed strategy focuses on scenarios that relieve the burden on hospitals, combined with reducing risks in the distribution of vaccines. Although the parameters are subject to change, we distinguish two scenarios:
- Hospitals are actively involved in the distribution chain. The Belgian distribution model envisages about 40 hospitals where interim storage and thawing (in the case of Pfizer and Moderna) takes place. From these hospitals, the 150 vaccination centers and other vaccination sites such as workplaces, residential care centers, etc. are supplied.
- Hospitals are excluded from the distribution chain and the vaccines are delivered directly to the national vaccination centers from a central hub.
The scenario in which hospitals take an active role seems to be a logical choice. At the same time, this creates additional activity in hospitals whose capacity is already under severe pressure. It is all the more likely that they will give priority to providing care rather than to preparing and distributing vaccines. And apart from the workload, additional operations and transports could also result in damage or loss of vaccines.
Workload and loss of vaccines
To build the scenarios respectively with and without hospitals, a number of known data and assumptions were used, as indicated in Annex 1. Two parameters were considered:
- Impact on hospital workload.
An FTE in a hospital can handle 1 500 vaccines per working day while for distribution workers in a central hub this is estimated at 3 000 vaccines. Handling involves the entirety of all operations: physical (receiving, stocking, chilling, thawing, shipping…) and administrative (preparation, planning, stock management, etc). - Impact on the loss of vaccines
In the scenario with hospitals as hubs, 3% loss of vaccines was assumed; in the scenario with a central hub, 2%. The loss rates were distributed taking into account the number of operations and the complexity of the activity. In the scenario without hospitals, the risk of hospital treatment and a transport activity is eliminated. Deliveries are made directly from a central hub to the vaccination center.
- Impact on hospital workload.
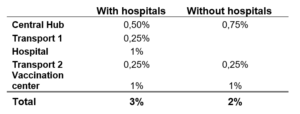
This is based on a number of studies that indicate that adding additional intermediate stops can increase the so-called ‘failure rate’ and ‘deterioration rate’ in refrigerated products. A study by Vogt (2010) shows that the two most important parameters in determining a hub are ‘suitability of building for logistics’ and ‘quality of personnel’ for performing logistics operations.
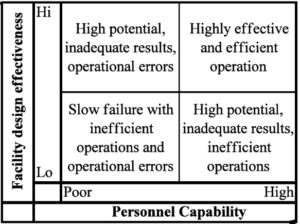
“We have absolutely no doubt about the quality of personnel in both hub hospitals and pharma logistics companies. However, we make the assumption that a hospital is not built to serve as a logistics hub where tens of thousands of vaccines per day need to be handled.”
Results
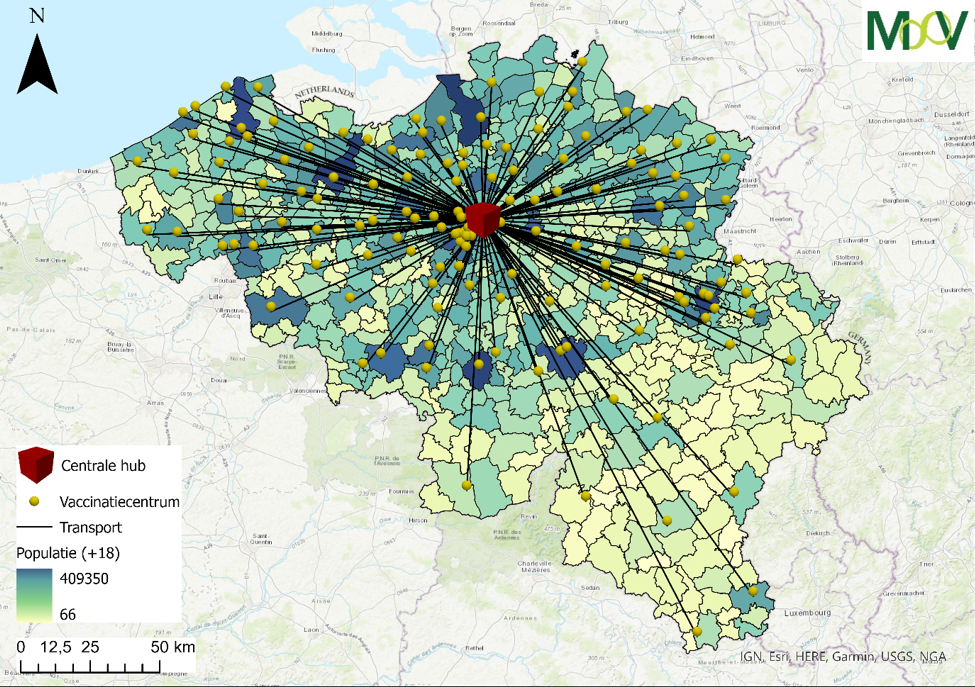
Both scenarios were calculated using the MooV optimization model. The model was developed by VITO and can solve complex distribution and supply chain scenarios. The figure below shows the scenario with hospitals (left) and the scenario without a hospital hub (right).
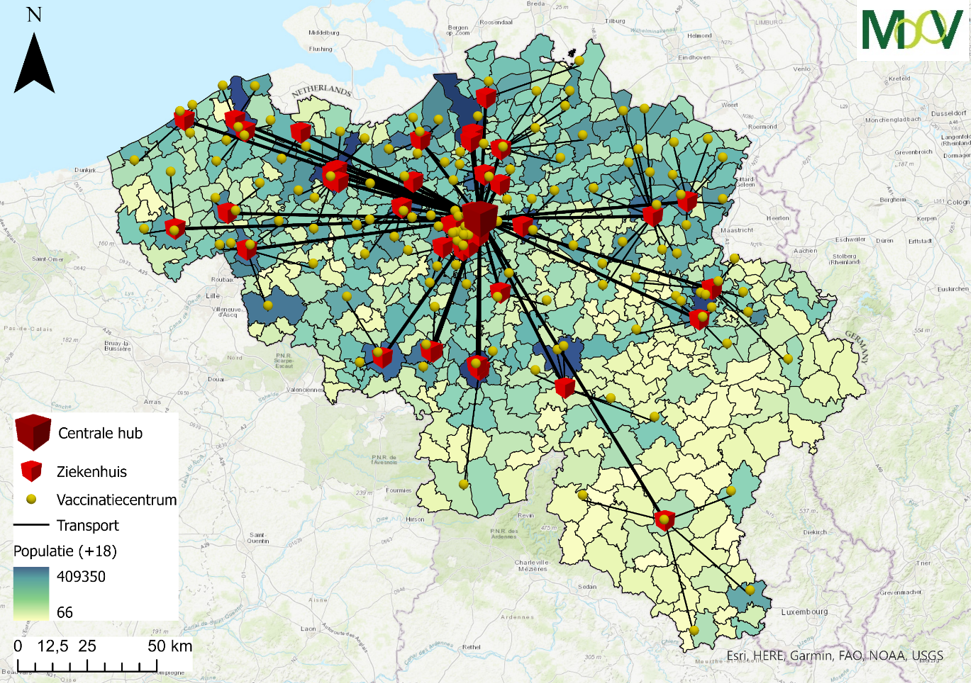
The results of the calculations based on the above assumptions show that in a scenario with hospitals, 140 hospital staff members are tasked with handling the vaccines on a full-time basis. These employees are therefore not available for care tasks. In the other scenario, vaccine handling is centralized in a central hub. The same tasks can be handled by about 50 additional specialized employees from the pharmadistribution sector.
In addition, in the scenario with hospitals, potentially 560,000 vaccines are lost across the campaign, compared to “only” 370,000 in the scenario with a central hub. This is a difference of 190,000 vaccines. Taking into account two vaccines per person, this means the equivalent of 95,000 protected persons or a medium-sized city.
Conclusions
Using hospitals as distribution hubs initially seemed a logical choice for storage and distribution of vaccines. However, the increased workload for the hospital staff (140 employees) and an increased risk of losing vaccines (190,000 vaccines) must be taken into account. Working with one central hub undeniably leads to better results.
However, a vaccination campaign on such a scale and a corresponding distribution strategy remains an absolute hurdle in both scenarios. There are still many uncertainties. In addition, variants of the discussed scenarios can also be calculated. We are thinking of not one but a limited number of central hubs in function of the respective vaccines or calculating the impact of a change in the choice and delivery of vaccines on the entire vaccination strategy.
Authors: Ruben Guisson (VITO), Annelies De Meyer (VITO), Roel Gevaers (UAntwerpen), Wouter Dewulf (UAntwerpen)
Annex 1
- The location of 1 hub centrally located in Belgium
- The location of the 40 largest hospitals – based on bed capacity
- The location of the vaccination centers
- The logistical cost of the vaccines (driving distance, driving time and loading and unloading time) both from central hub to the hospitals and from the hospitals to the vaccination centers
- The logistics cost of the people – the trip to the vaccination center
- The number of vaccines available per month – pro rata taking into account planned delivery times of the five main vaccines (AstraZeneca, Curevac, J&J, Moderna, and Pfizer)
- The storage conditions – specifically Pfizer (-70°C) and Moderna (-20°C)
- The number of people in the vaccination centers that each hospital must supply – calculated from population figures (StatBel)
- Order of vaccination with priority vaccination of people aged 65+ and at risk groups
- A vaccination time horizon up to and including October 2021
- The need for a second vaccination – a few weeks after the first one
- An active regime of 7/7 in the hospitals
- A work regime of 5/7 of hospital staff