Prof. Guy Caljon from the Laboratory of Microbiology, Parasitology and Hygiene (LMPH).
Understanding how pathogens survive is key to fighting infectious diseases. One such survival tactic, quiescence, makes it challenging to treat diseases like leishmaniasis. Leishmaniasis is a disease caused by Leishmania parasites, transmitted through the bites of infected sand flies, and it can affect the skin, mucous membranes, and internal organs.
Quiescence is a dormant state where cells or organisms slow down or stop their growth and division to conserve energy and resources. In this state, they become resistant to environmental stresses, including drug treatments. For Leishmania parasites, entering quiescence allows them to evade antiparasitic drugs, leading to potential treatment failures and relapses. Understanding quiescence is crucial for developing more effective treatments for infectious diseases.
Recent research conducted by Prof. Guy Caljon and Dr. Laura Dirkx from the University of Antwerp has shed light on this behavior in Leishmania parasites, offering insights that could improve future treatments.
Dr. Laura Dirkx studying Leishmania parasites.
Leishmania infantum and L. donovani are parasites that cause leishmaniasis, affecting millions of people worldwide. Prof. Guy Caljon’s team found that these parasites enter a quiescent state quickly after just 2-3 cell divisions when in human and mouse bone marrow stem cells. Interestingly, this quiescence doesn’t happen in macrophages, the main cells infected by Leishmania.
When Leishmania parasites enter quiescence, their gene activity drops significantly. This reduced activity is a hallmark of quiescence, with the parasites essentially “shutting down” their metabolism. In this state, the parasites are smaller and show signs of rapid genetic adaptation, helping them to survive tough conditions.
Quiescence makes Leishmania parasites much harder to treat. In their dormant state, they resist antiparasitic drugs, leading to treatment failures. Additionally, this state helps the parasites spread via sand flies, the insects that transmit leishmaniasis. Quiescent parasites are better at infecting new cells, increasing the risk of disease spread.


Sandflies infected with the Leishmania parasites are used to study Leishmaniasis.
Moving Forward
This study has identified bone marrow stem cells as a key place where Leishmania enters quiescence. Tackling Leishmania’s quiescent state is crucial for better treatment outcomes. Future research will focus on uncovering the molecular mechanisms of quiescence and finding ways to target this phase effectively. This could lead to more robust treatments that prevent relapse and control the spread of leishmaniasis.
Prof. Guy Caljon explains, “Our discovery of Leishmania’s quiescent state in bone marrow stem cells opens up new avenues for targeted treatments. This could significantly improve how we manage this disease.” Dr. Laura Dirkx adds, “By understanding the quiescent behavior of these parasites, we can develop strategies to disrupt their survival tactics, leading to more effective therapies.”

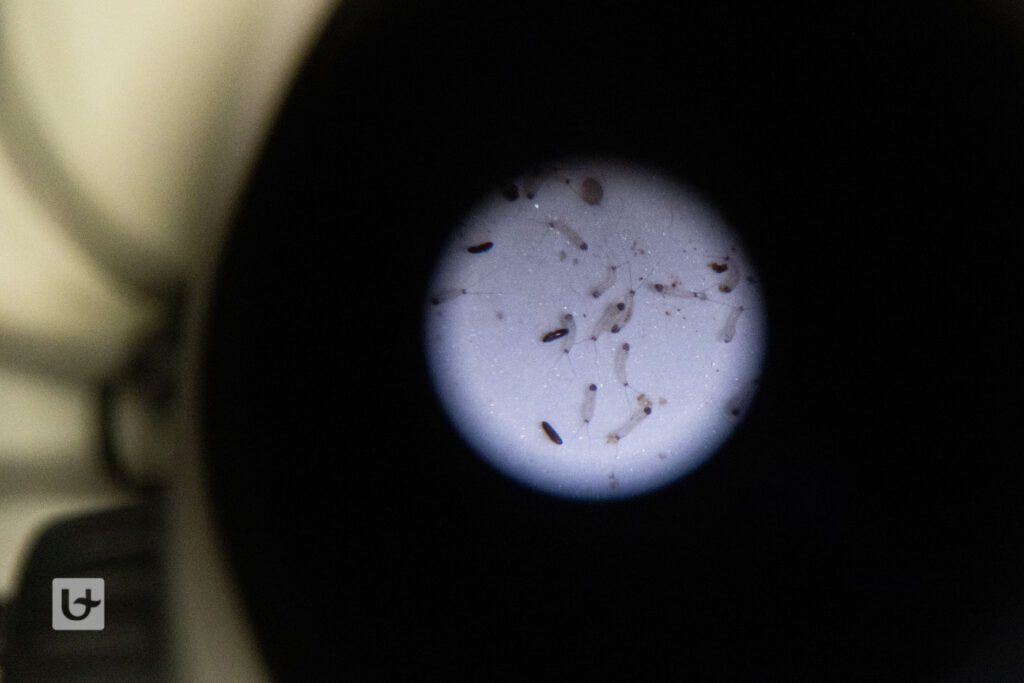
Sand fly larvae viewed under the microscope.
In another recent study in collaboration with Prof. Johan van Griensven and Dr. Myrthe Pareyn at the Institute of Tropical Medicine (ITM) in Antwerp and with the University of Gondar Hospital and Arba Minch University in Ethiopia, Prof. Caljon’s group investigated how to effectively monitor treatment response in visceral leishmaniasis. Traditional methods like microscopic tissue examination have drawbacks due to invasiveness and limited sensitivity. To address this, Prof. Caljon’s team compared two molecular markers: kDNA and SL-RNA, to assess parasite viability. While kDNA persists post-parasite death, SL-RNA rapidly degrades, proving to be a superior real-time indicator of viability. Moreover, SL-RNA levels closely correlated with microscopic observations, enhancing accuracy. This advancement holds significant clinical implications, allowing for earlier assessment of treatment efficacy, thus facilitating tailored patient care and improving outcomes.
Thus, identifying Leishmania‘s rapid entry into quiescence within bone marrow stem cells and its absence in macrophages highlights a critical survival strategy. This knowledge paves the way for new treatments aimed at disrupting quiescence, offering hope for better management of this persistent parasite. Additionally, it was shown that SL-RNA quantitative PCR represents a superior tool for treatment monitoring, offering personalized patient management and early efficacy evaluation in clinical trials.
Article written by Dr. Bronwen Martin. Photos by Teun De Voeght.