Prof. Jean-Pierre Timmermans, Dr. Peter Verstraelen and Prof. Winnok De Vos.
A new study by Dr. Peter Verstraelen, Prof. Jean-Pierre Timmermans, and Prof. Winnok De Vos from the Laboratory of Cell Biology and Histology and an international team of collaborators has revealed novel insights into how gut bacteria might influence our immune system and brain health. By gaining a better understanding of these processes, early diagnosis and treatment of various diseases could be improved.
Understanding Gut Inflammation
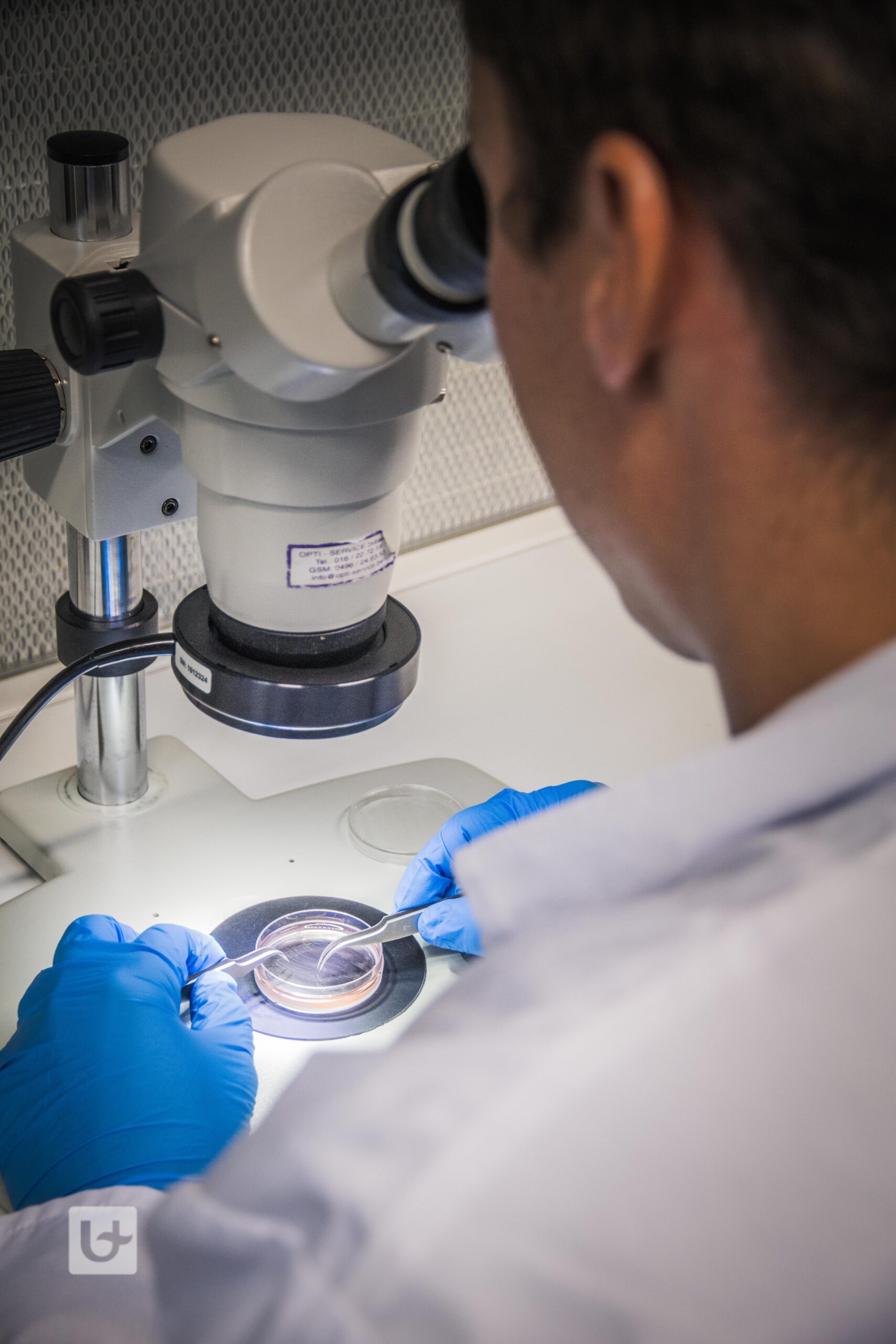
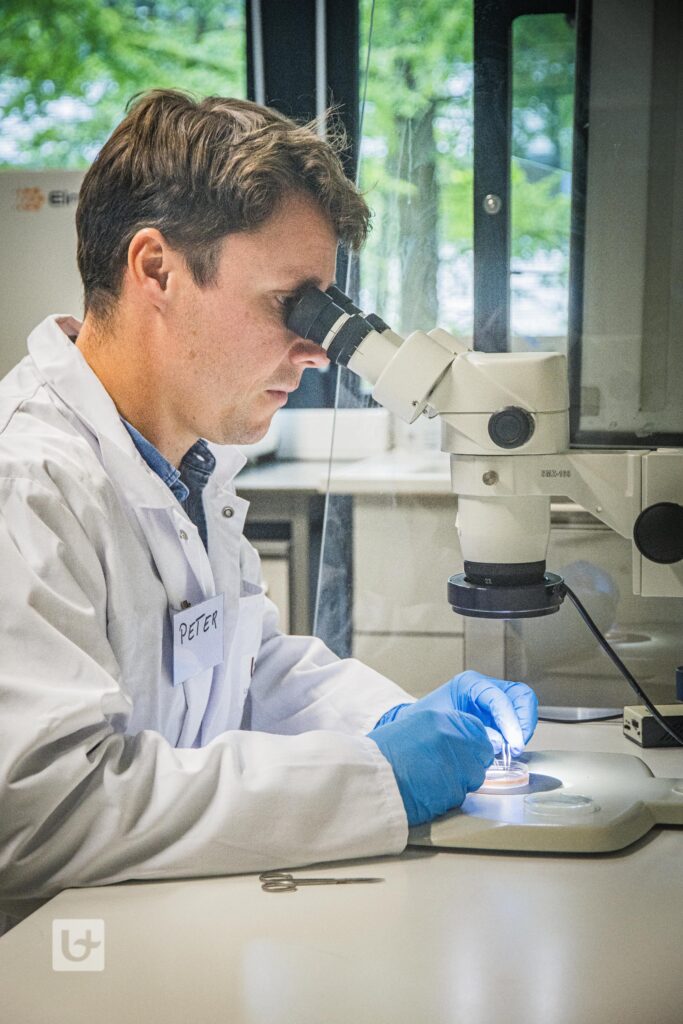
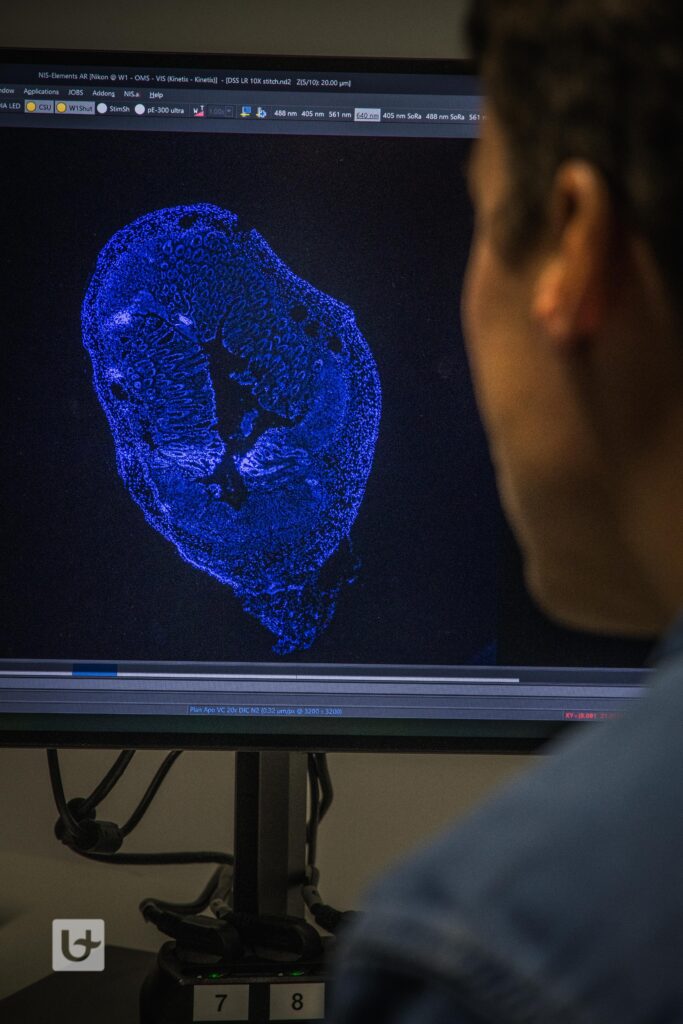
This research focused on curli, a protein commonly produced by bacteria that helps them stick to surfaces and form biofilms. The team exposed mouse gut nerve cells to curli and observed the changes using advanced genetic and biochemical techniques. They also tested the effects of curli in live mice by injecting it into their colon walls.
The study found that curli caused a strong inflammatory response in the gut, particularly affecting glial cells, which are support cells in the nervous system. This inflammation increased the production of a protein called Serum Amyloid A3 (SAA3), which is involved in the body’s early defense system against infections. The rise in SAA3 led to an influx of immune cells and caused DNA damage (changes in DNA structure that can lead to cell malfunction) and cell replication (the process by which cells divide and multiply). When the researchers added SAA3 alone, it mimicked the inflammatory response seen with curli. Conversely, removing SAA3 reduced the damage caused by curli. Additionally, infections with curli-producing bacteria and colon inflammation also increased SAA3 levels, indicating its key role in gut health problems.
Furthermore, the study also showed that blocking a specific enzyme called dual leucine zipper kinase, which plays a crucial role in the body’s stress responses, reduced the harmful effects of curli and SAA3, including inflammation and DNA damage.
New Avenues for Treatment
“This study highlights the critical role of SAA3 in gut inflammation caused by bacterial proteins” explains Dr. Peter Verstraelen. “We will now further investigate whether this protein enters the bloodstream and the brain, where it could affect the progression of dementia”.
Although these hypotheses need to be experimentally verified, understanding how bacterial proteins like curli trigger gut inflammation opens new possibilities for treating diseases related to gut health and potentially even brain diseases at an early stage. By targeting specific enzymes like dual leucine zipper kinase, we may be able to mitigate the harmful effects of bacterial proteins and improve overall health outcomes.

About Dr. Peter Verstraelen
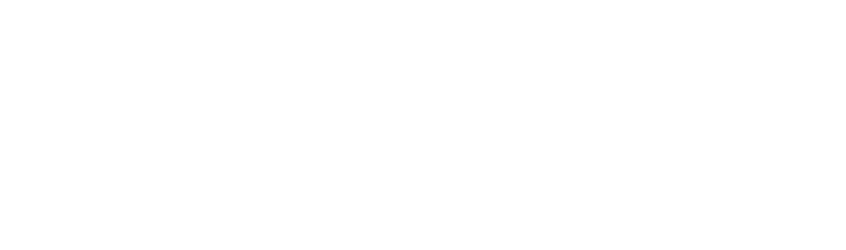
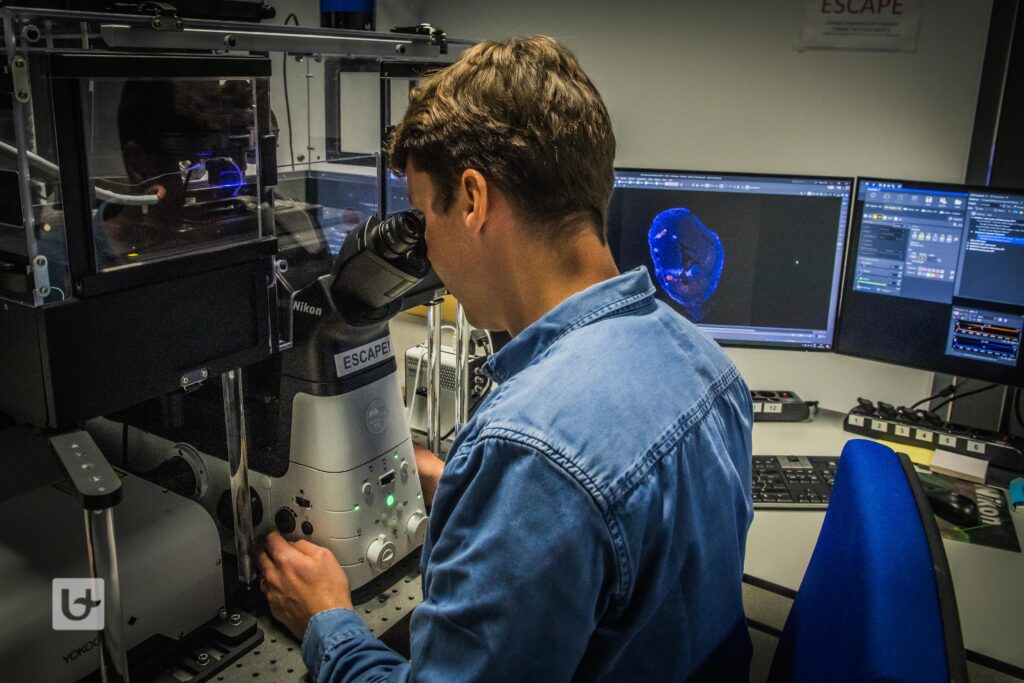
Dr. Peter Verstraelen is an expert in studying the role of the microbiome-gut-brain axis in neurodegeneration using in vitro (test tube or cell culture), ex vivo (outside the living organism), and in vivo (within the living organism) preclinical models. His extensive research focuses on how the interactions between gut bacteria and the nervous system affect brain health and disease.
Further reading
https://www.cmghjournal.org/article/S2352-345X(24)00113-9/fulltext
https://www.uantwerpen.be/en/research-groups/celw
Article written by Dr. Bronwen Martin. Photos by Teun De Voeght.